 Derek Maylor, NW BT Unions H&S Co-ord member and Health & Safety Officer (Telecom section) of the CWU's Grter Mersey Amal Branch; reports on this Covid-19 event by the Royal Society Of Medicine which he attended via video conference on 19th November:
Derek Maylor, NW BT Unions H&S Co-ord member and Health & Safety Officer (Telecom section) of the CWU's Grter Mersey Amal Branch; reports on this Covid-19 event by the Royal Society Of Medicine which he attended via video conference on 19th November:
Dr Ebere Okereke, Consultant in Global Public Health for PHE led the discussion with Dr John Nkengasong, Director of the Africa Centers for Disease Control and Prevention, Dr Magda Robalo, Minister in the Office of the President and High Commissioner for COVID-19 for Guinea-Bissau, and
Dr Chikwe Ihekweazu, Director General of the Nigeria Centre for Disease Control.
Focusing on the pandemic in Africa and key successes and challenges to see what we can learn from the response where the virus has been managed alongside other epidemics like ebola and cholera.
 According to the WHO sub-Saharan Africa has only 3% of the world’s health workers who have to look after 11% of the world population, which also has over 25% of the global disease burden. It was noted in 2014 that a pandemic would threaten to overwhelm health infrastructure so there was a need to unite, and they did.
According to the WHO sub-Saharan Africa has only 3% of the world’s health workers who have to look after 11% of the world population, which also has over 25% of the global disease burden. It was noted in 2014 that a pandemic would threaten to overwhelm health infrastructure so there was a need to unite, and they did.
At the beginning of the pandemic, a lot of Western experts were prediction catastrophic outcomes for all African countries but they hadn’t considered previous experiences with other epidemics (such as ebola 2014 & 2016) had put them ahead of European countries in the experience needed to deal with it.
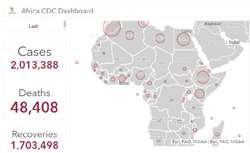
There have been consistent low morbidity and mortality is significantly lower than North America and Europe, nevertheless there have been two million cases across Africa. Note that the whole of Africa has had fewer deaths than the UK alone. There has been extraordinary leadership and population adherence to urgent and sudden requirements such as wearing masks, politically there have been defined strategy and a joined up approach with a task force from the beginning.
There have been nine meetings of the leaders of all counties with one item on the agenda to target a unified response. The collective response was a major difference to that of countries in Europe which, despite the EU, was each country on its own and even state by state within that response. COVID-19 was seen as a political issue not just a health issue, needing a political response and borders were closed quickly, 18th March, decisive action was taken ASAP.
There was an explosive outbreak in Nigeria but it was contained, a lock down in Lagos was fully accepted and supported by the population almost overnight. Although there were a lot of unknowns they took what they did know and acted.
Africa and the world are not out of the pandemic yet and the economic impact of a near shutdown of a countries economy will be felt for years. However the whole effort and focus went into in public health and this has been a shining example. It could be said that some Western countries were prioritising the economy before the population’s health. There needs to be further development of local public health systems that are already there, far better placed to react to situations at speed than a national policy pushed down to implement, though the parameters were set by the continent.
At the beginning the richest economies around the world looked after themselves, buying too much PPE which was not all needed, this also pushed up the price of PPE (but they had theirs); many were pre-buying drugs that have not even been developed for themselves and so on, nationalism first. African countries were a long way down the list of concerns. Magnanimously it was said that when the pandemic dust settles there needs to be uncomfortable discussions over the world’s health and suitable and sufficient funding of the WHO.
We have the current waves of announcements of new vaccines and if they are proved to be effective there should be a fair distribution of these resources not just going to the highest bidder. The legacy for future antiviral treatments should be that we, as a global health community, ensure that there is a fair distribution of these resources.
The organisation Africa CDC (Africa Centre for Disease Control & Prevention) may not a lot of resources but they appear to manage well what they do have and lead the solidarity between the African countries which have been enhanced by the reaction to the pandemic.
 In our lifetimes there was a HIV pandemic, 12,000,000 Africans died and most of these deaths were when there was treatment available but at a cost of $10k per patient per year – Africans could watch patients in Europe and America on TV getting treatment yet they could not access the same safety treatment for themselves or their family.
In our lifetimes there was a HIV pandemic, 12,000,000 Africans died and most of these deaths were when there was treatment available but at a cost of $10k per patient per year – Africans could watch patients in Europe and America on TV getting treatment yet they could not access the same safety treatment for themselves or their family.
* The international community should support Africa's countries to being self-sufficient in developing their own healthcare tools, drugs and sustainable scientific support that enables independence to prevent African nations being reliant and subservient to others.
* If European countries had unified and acted together like the whole of Africa there would have been fewer deaths.
* If countries had acted like the African countries in putting public health before money there would have been fewer deaths.
* If countries had not, as they continue to do so, raced each other in the rush to buy their own safety at the expense of others there would have been fewer deaths.
For further information:
https://africacdc.org/ and www.rsm.ac.uk/


 Derek Maylor, NW BT Unions H&S Co-ord member and Health & Safety Officer (Telecom section) of the CWU's Grter Mersey Amal Branch; reports on this Covid-19 event by the Royal Society Of Medicine which he attended via video conference on 19th November:
Derek Maylor, NW BT Unions H&S Co-ord member and Health & Safety Officer (Telecom section) of the CWU's Grter Mersey Amal Branch; reports on this Covid-19 event by the Royal Society Of Medicine which he attended via video conference on 19th November: According to the WHO sub-Saharan Africa has only 3% of the world’s health workers who have to look after 11% of the world population, which also has over 25% of the global disease burden. It was noted in 2014 that a pandemic would threaten to overwhelm health infrastructure so there was a need to unite, and they did.
According to the WHO sub-Saharan Africa has only 3% of the world’s health workers who have to look after 11% of the world population, which also has over 25% of the global disease burden. It was noted in 2014 that a pandemic would threaten to overwhelm health infrastructure so there was a need to unite, and they did.